5 Thyroidectomy Complications and How To Manage Them

If you’ve been told that you need a thyroidectomy, you likely have some concerns about the procedure. First, rest assured that thyroidectomies have a very low rate of complications.
But as with any procedure, complications do sometimes occur. Today we’re taking a look at the five most common thyroidectomy complications and how to deal with each of them.
What Is a Thyroidectomy?
A thyroidectomy is a surgery to remove part or all of the thyroid gland that sits at the base of your neck.
The thyroid gland sits in front of your voice box and is shaped like a butterfly, with two lobes connected in the middle by an isthmus. It makes and releases thyroid hormones into your bloodstream, playing an important role in many vital body functions like heart rate, temperature level, energy level, and metabolism.
When the thyroid doesn’t function properly, it can lead to problems that may make a thyroidectomy necessary. Some conditions that may require a thyroidectomy include:
- Overactive thyroid (hyperthyroidism).
- Thyroid cancer.
- Suspicious nodules.
- Goiter (noncancerous thyroid enlargement).
Possible Thyroidectomy Complications
Although a thyroidectomy is a fairly straightforward and routine procedure, a few complications can sometimes arise after surgery. We’ll address them here from most common to least common.
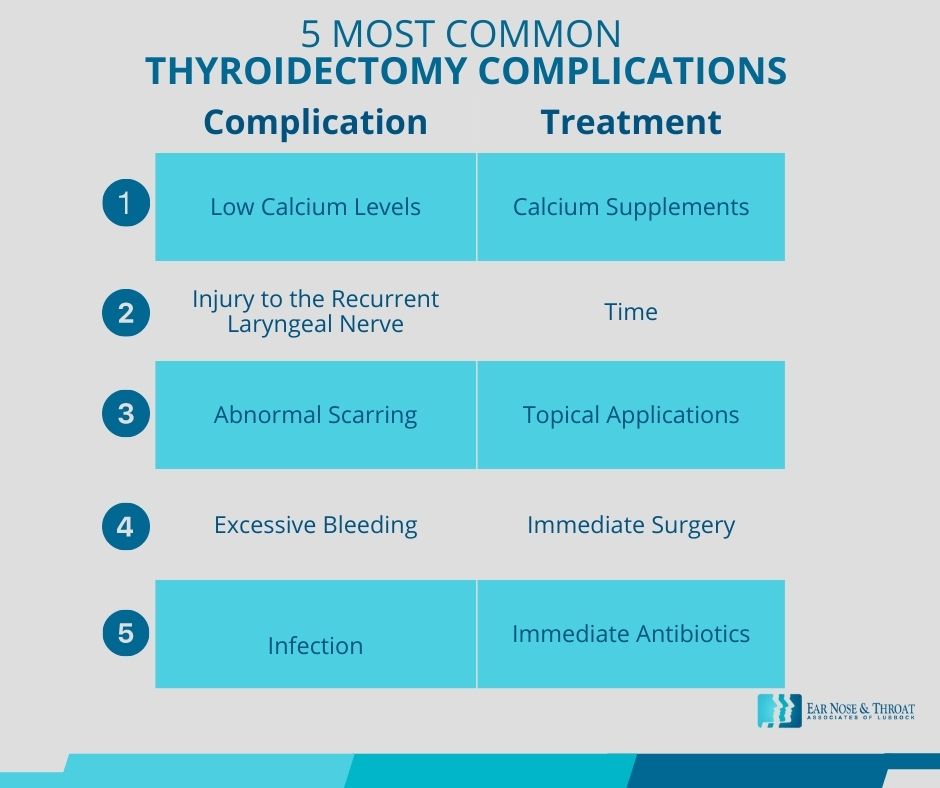
1. Low Calcium Levels
A low calcium level, also known as hypocalcemia, is the most common thyroidectomy complication. Behind the thyroid are four small glands called the parathyroid glands. Sometimes after a thyroidectomy, your parathyroid glands experience a kind of “shock” and don’t function properly for a short time due to inflammation.
This parathyroid shock results in not enough parathyroid hormone being released into the body and causes transient hypocalcemia, a temporary reduction in the calcium levels in your blood. It is common after a complete (versus partial) thyroidectomy, particularly when the thyroid gland is extremely enlarged, as with Graves’ disease.
Because hypocalcemia is so common, we recommend that our patients take calcium tablets like Tums for a few weeks after their thyroidectomy to make sure their calcium levels stay within normal range. You can also supplement with vitamin D to ensure the calcium is well absorbed.
2. Injury to the Recurrent Laryngeal Nerve
Because the recurrent laryngeal nerve is so close to the thyroid gland, it can be easily damaged during a thyroidectomy. Damage to this nerve can cause vocal cord problems (paresis) and difficulty breathing and swallowing.
Talk to your doctor if you find that your voice is hoarse or you experience trouble with breathing or swallowing after your thyroidectomy. In most cases the injury resolves itself with time — usually several months — but some surgical treatments are available if necessary.
This complication is much less common with high-volume surgeons, which is why we recommend seeking out an experienced, high-volume surgeon for your thyroidectomy.
3. Abnormal Scarring
Most thyroidectomy incisions now are significantly smaller than they were in past years, so there is less opportunity for scarring. Your grandmother’s thyroid scar, for instance, may have been long and curvy across her whole upper chest, but a thyroidectomy scar today is usually short and straight across the lower neck.
Surgeons close thyroidectomies in the same way that plastic surgeons close face lift and breast augmentation incisions. They place the stitches underneath the skin, and only thin, adhesive bandages remain outside.
The best way to avoid abnormal scarring is to follow your surgeon’s postoperative instructions. But some people’s skin is simply more prone to abnormal scarring, such as hypertrophic or keloid scarring, than others. If you develop an abnormal scar, you can talk to your doctor about topical treatments, scar injections, or scar-reduction surgery.
4. Excessive Bleeding
Excessive bleeding after thyroidectomy surgery is extremely rare, and having an experienced, high-volume surgeon makes it even more rare. This complication will most likely appear while the patient is still in recovery at the surgery center.
Excessive bleeding after a thyroidectomy is a serious complication that can require a return to surgery. If you’re taking blood thinners like aspirin or warfarin before surgery, it’s important to ask your surgeon how long prior to surgery you need to stop taking these medications.
5. Infection
Unfortunately, infection is a risk any time a surgical incision is made on the body. The good news is that the neck has excellent blood flow, so infection following a thyroidectomy is unusual. Infection is a more rare complication even than bleeding.
When it does happen, though, post-surgical infection usually arises a few days after surgery. Signs of infection usually include redness and swelling around the incision. You should contact your doctor immediately if you think your surgical site might be infected.
Infection can be treated with antibiotics, but sometimes drainage may also be necessary.
A Tip for a Complication-Free Thyroidectomy Recovery
One of the most important recommendations we can give about thyroidectomy recovery is to follow your ENT surgeon’s postoperative instructions. Be sure to keep your follow-up appointments as well, so your healthcare team can help you be proactive in spotting any abnormalities.
The physicians at ENT Associates of Lubbock are high-volume thyroid surgeons, performing multiple thyroidectomies every week. Call ENT Associates of Lubbock today to schedule a consultation. We’ll be happy to answer any questions you have and will be by your side throughout your recovery.
Dr. Scolaro is a board-certified Otolaryngologist servicing the South Plains area. He has been practicing in Lubbock since 1990 and has earned a reputation as a skilled and experienced surgeon. He currently serves as the Medical Director for Covenant High Plains Surgery Center campuses, is a member of Covenant Health Partners and is an adjunct faculty professor for Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro.
Categories: